Out of an abundance of caution, US officials on Tuesday recommended pausing use of Johnson & Johnson’s COVID-19 vaccine. Officials linked the vaccine to six peculiar illnesses in which people developed life-threatening blood clots in combination with low levels of blood platelets, the cell fragments in blood that form clots. One person died from their condition and another is in critical condition.
It’s unclear if the vaccine caused the illnesses. Even if it did, the illnesses would represent an exceedingly rare side effect. The six cases occurred among more than 6.8 million people in the US who received the Johnson & Johnson vaccine. That would make it a side effect seen in fewer than one in a million. The risk of hospitalization and death from COVID-19, which the vaccine protects against, easily exceeds those odds. Without question, the benefits of the vaccine outweigh the potential risks.
Still, with robust supplies of vaccine from Moderna and Pfizer-BioNtech—neither of which have been linked to these unusual cases—US officials took the cautious route of pausing Johnson & Johnson’s vaccine while they investigate the cases further and inform clinicians about how to spot and treat any others that may arise. This latter point is critical, because if doctors try to use standard blood clot treatments in these vaccine-linked cases, the outcomes can be fatal.
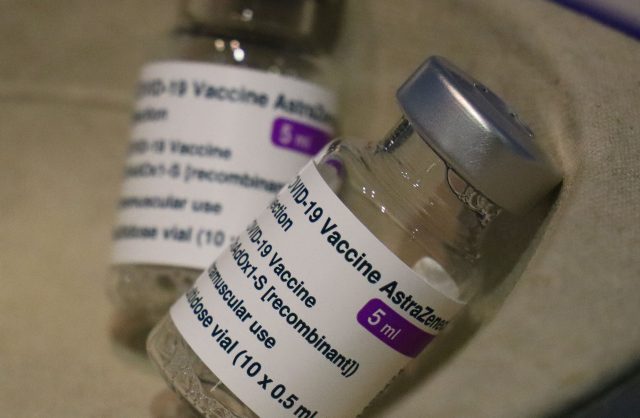
Of course, the other critical aspect of this situation is that officials have seen these unusual cases before—linked to a similar COVID-19 vaccine developed by AstraZeneca and researchers at the University of Oxford. The AstraZeneca vaccine is not yet authorized for use in the US, but it has been authorized in many other countries, including those in the European Union. In recent weeks, regulators in the EU and the UK have investigated dozens of eerily similar cases, involving dangerous blood clots coupled with low platelets. Some estimates have pegged the reported case rate of one in 100,000 people vaccinated.
Trying now to connect all the dots and find answers, experts are eyeing the most obvious connection: both vaccines use an adenovirus vector, a viral delivery system used regularly in vaccine development.
At the moment, the adenovirus vector offers “the most straightforward explanation” for the possible side effects, says viral immunologist Hildegund Ertl, who develops adenovirus-based vaccines at the Wistar Institute in Philadelphia. Yet, the link to blood clots “took all of us by surprise,” she tells Ars. The situation has raised a slew of questions—as well as some doubts.
Vexing virus
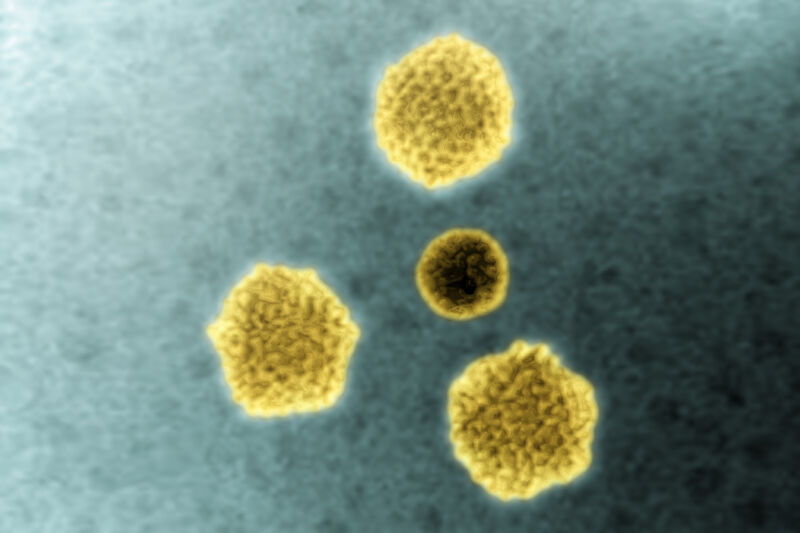
Adenoviruses are a large family of very common viruses that cause a range of infections in humans, from mild colds and flu-like illnesses to pink eye, pneumonia, and gastroenteritis. Beyond humans, they can infect a range of animals, including pigs, cows, and chimpanzees. Researchers have been working with adenoviruses for decades. The Johnson & Johnson vaccine uses the adenovirus (Ad26), which was first identified in 1961 from anal swabs of children in Washington, DC. The AstraZeneca vaccine is based on an adenovirus that circulates in chimpanzees (ChAdOx1).
Over the years, researchers have considered adenoviruses useful delivery systems for vaccines and gene therapies. For starters, they’re easy to brew up in big batches in laboratory conditions. When engineered for vaccines, they can provoke potent immune responses in people against germs we want to fight. And they appeared relatively safe in humans, particularly since they’re often modified so they can’t replicate in our cells.
But adenoviruses have had a troubled past. Researchers all but abandoned their use in gene therapies in 1999 following the tragic death of 18-year-old Jesse Gelsinger. A team of researchers at the University of Pennsylvania had hoped to cure the teenager’s rare metabolic liver disease by correcting an underlying genetic mutation with new code—delivered in trillions of adenovirus vectors. The researchers used human adenovirus 5 (Ad5), which typically causes only a mild cold. In early tests, the therapy triggered only mild side effects and flu-like symptoms in animals and a human patient, The New York Times reported at the time. But in Gelsinger, the massive dose of virus vectors triggered a fatal immune response.
Researchers carried on with adenoviruses for vaccine development, where potent immune responses can be a plus instead of a peril. Programmed to be vaccine vectors, adenoviruses deliver key snippets of genetic code from dangerous viruses, bacteria, or parasites directly to human cells. From there, our cells translate the genetic code into protein, recognize it as foreign, and use it to train our immune systems to seek and destroy anything carrying the same protein. In the case of COVID-19, adenovirus-based vaccines carry the genetic code for the SARS-CoV-2 spike protein, which is the thorny protein that juts from the virus’s particle. The spike protein is what SARS-CoV-2 uses to enter human cells, and it's a key target for potent antibodies and other immune responses.
Shaky shots
Adenovirus-based vaccines have held a lot of promise over the years, but they have had notable stumbles, too. Nearly a decade after Gelsinger’s death, researchers halted a major trial of an Ad5-based HIV vaccine after data indicated that the vaccine increased the risk of becoming infected with HIV in people who had preexisting immune responses to Ad5. With the high-profile failure, many vaccine developers moved away from Ad5 to other adenoviruses—ones that people tend to have less preexisting immunity against, like chimpanzee adenoviruses.
Though researchers have been developing adenovirus-based vaccines against a slew of diseases—malaria, HIV, Zika, RSV (respiratory syncytial virus), and more—few have made it across the finish line and into use. Among the most successful is an Ad26-based Ebola vaccine made by Johnson & Johnson, which gained regulatory approval in Europe last year. The approval bolstered hopes for the company’s COVID-19 vaccine, which uses the same Ad26-based platform.
Early on in the pandemic, the adenovirus-based vaccines were often seen as front-runners, particularly AstraZeneca’s. Despite the checkered past of adenovirus vectors, the vaccine design was seen as a more established technology than the mRNA-based vaccines, which were completely unproven until the extraordinary success of COVID-19 vaccines from Moderna and Pfizer-BioNTech. Adenoviruses also have logistical advantages. They’re relatively cheap, easy to make, and easy to distribute. For instance, unlike the mRNA vaccines, which require ultra-cold storage conditions, AstraZeneca’s vaccine can handle normal refrigerator temperatures. Many experts and the World Health Organization have considered AstraZeneca’s vaccine to be the world’s go-to vaccine—a cheap, accessible vaccine that could be used in a variety of countries and settings.But as the mRNA vaccines sprinted ahead in the pandemic, AstraZeneca seemed to lurch from problem to problem. The vaccine’s troubles hit a critical point last month when more than a dozen countries temporarily suspended its use amid concerns that it was causing extremely rare blood clots. On April 7, an investigation by the EU’s European Medicines Agency concluded that there was a strong association between the vaccine and peculiar illnesses involving both blood clots and low platelets. The agency determined that they should be listed as “very rare side effects” of the vaccine, but it still urged countries to continue using the vaccine.
“The reported combination of blood clots and low blood platelets is very rare,” the agency noted. “The overall benefits of the vaccine in preventing COVID-19 outweigh the risks of side effects.”
Confusing clots
For its investigation, EMA reviewed 86 cases of blood clots among around 25 million people who received AstraZeneca’s vaccine in Europe and the UK. Sixty-two of the cases were diagnosed as cerebral venous sinus thrombosis (CVST), a rare form of stroke in which a clot prevents blood from draining out of the brain. The remaining 24 cases were diagnosed as splanchnic vein thrombosis, in which blood clots develop in veins that drain blood from the abdomen. Of those 86 cases, 18 people died.
As researchers had done before, the regulators noted the unusual combination of blood clots and low platelets. Having low platelets typically leads to increased bleeding, not increased clotting. But the combination was not entirely unheard of: it closely resembles a condition called heparin-induced thrombocytopenia or HIT. The condition arises rarely in people who are given heparin, which is an anticlotting drug. In these rare cases, heparin use backfires, leading to a drop in platelets and a hyperclotting state, which can lead to widespread clotting and death.
Researchers have already worked out that HIT develops because of an aberrant immune response. In a reaction to heparin that scientists don’t entirely understand, some patients start producing antibodies that attack a common platelet protein called Platelet Factor 4, or PF4. These antibodies seem to activate platelets and pro-clotting particles, while lowering platelet levels, ultimately leading to HIT.
Researchers quickly drew a connection between HIT and the blood clots seen with AstraZeneca’s vaccine, suspecting a similar berserk immune response. In an early study of patients who developed blood clots after vaccination, 28 patients tested positive for antibodies against PF4–heparin, even though none of them had been treated with heparin before becoming ill. They also all tested positive for platelet activation. The study authors, led by researchers in Germany, suggested that the immune reaction could be treated with nonheparin anticlotting drugs as well as a high dose of immune globulin, which has been shown to raise platelet counts and inhibit hyperclotting in HIT patients.
Common suspect
Though the data provides paths forward for more research and potential treatments, experts remain puzzled over how the vaccine might be causing a HIT-like condition in a very small number of patients. As viral immunologist Ertl at the Wistar Institute noted, the adenovirus vector was the obvious first suspect.
Researchers had noted years before that several adenoviruses can bind to platelets and activate them. In animal studies using adenoviral vectors for gene transfers, researchers had even seen the vectors trigger platelet activation and low platelet levels. That said, the small batch of adenovirus vectors delivered in a vaccine shot is unlikely to stick around and cause significant platelet activation seen in patients one or two weeks after their vaccination. But, researchers still say it’s possible that the interaction between the adenovirus vector and platelets, or PF4 specifically, could play some role in the unusual cases.
The German researchers who studied some of the early HIT-like cases have also speculated that the adenoviral vaccine’s DNA code could be the trigger. In their study, published in the New England Journal of Medicine, they note that they “have previously shown that DNA and RNA form multimolecular complexes with PF4, which bind antibodies from patients with heparin-induced thrombocytopenia and also induce antibodies against PF4–heparin in a [mouse] model.”
Still, Ertl has some doubts about these hypotheses. “Adenoviruses are extremely common and we have more than 50 serotypes that can infect humans,” she notes to Ars. “Most humans get adenoviruses over and over and over.” In all of her research and literature searches, she found no references of these blood clots after natural adenovirus infection. “So that makes me wonder about this particular explanation… Why on Earth does this only happen after you give it as a vaccine, but not after a natural infection?”
The hypothesis seemed to carry a little more weight after Tuesday, when US officials announced the six cases in connection with Johnson & Johnson’s vaccine—another adenovirus-based vaccine.

Class questions
Though researchers have been on the lookout for other HIT-like conditions across all of the vaccines, use of Johnson & Johnson’s vaccine has lagged behind use of AstraZeneca’s vaccine and that of the mRNA vaccines. In a press briefing April 7, Peter Arlett, the head of data analytics at the EMA, said there was an early sign of an increased risk of these blood-clotting conditions in Johnson & Johnson’s clinical trial, but the trial wasn’t able to confirm or disprove the link. Even the largest clinical trials aren’t large enough to detect extremely rare side effects that may crop up in one-in-a-million people.
In this case, it may not just be about the numbers, however small they are, said Peter Marks, the top vaccine regulator with the Food and Drug Administration, during a press briefing Tuesday. We can look at background rates of clotting conditions like CVST and background rates of low blood platelets, Marks said. But “it’s their occurrence together that makes a pattern and that pattern is very, very similar to what was seen in Europe with another vaccine.”
When pressed to say whether these blood clotting conditions could be a risk for all adenovirus-based vaccines, Marks was uncertain but left the idea standing. “I hesitate to call it a class effect,” he said. “But I think it’s plainly obvious to us already that what we’re seeing with the Janssen [Johnson & Johnson] vaccine looks very similar to what was being seen with the AstraZeneca vaccine… The AstraZeneca vaccine is a chimpanzee adenoviral vector vaccine, the Janssen is a human adenoviral vector. So, I can’t make some broad statement yet, but obviously they are from the same general class of viral vectors.”
Ertl was more skeptical, saying that she’d like to see more data on the vaccines and their link to the cases. She noted that AstraZeneca and Johnson & Johnson are not the only companies with adenoviral-based COVID-19 vaccines in use. China’s CanSino vaccine and Russia’s Sputnik V vaccines also use adenoviruses (Ad5, and an Ad5/Ad26 combination, respectively). It’s unclear if those vaccines are also being linked to these unusual clotting disorders.
But even if the clotting conditions are due to the adenovirus vectors, Ertl emphasizes that the risk is still extremely small, the vaccines should still be used, and there’s hope for adenoviral vectors ahead.
“Adenoviruses have taken a lot of hits in their lifetime,” she laughed. “I think we will find out a lot fairly rapidly… There is so much motivation right now to figure out what’s going on. I think they’ll get answers reasonably soon,” she said. “And once we know what’s causing it, I am very confident that we can fix it.”